-
Epidemics That Didn't Happen
-
LATEST CASE STUDIES
-
FLAGSHIP REPORTS
EpidemicsThat Didn'tHappen
In a series of flagship reports and standalone case studies, Resolve to Save Lives highlights the inspiring stories of outbreaks that were stopped in their tracks through swift and effective action.
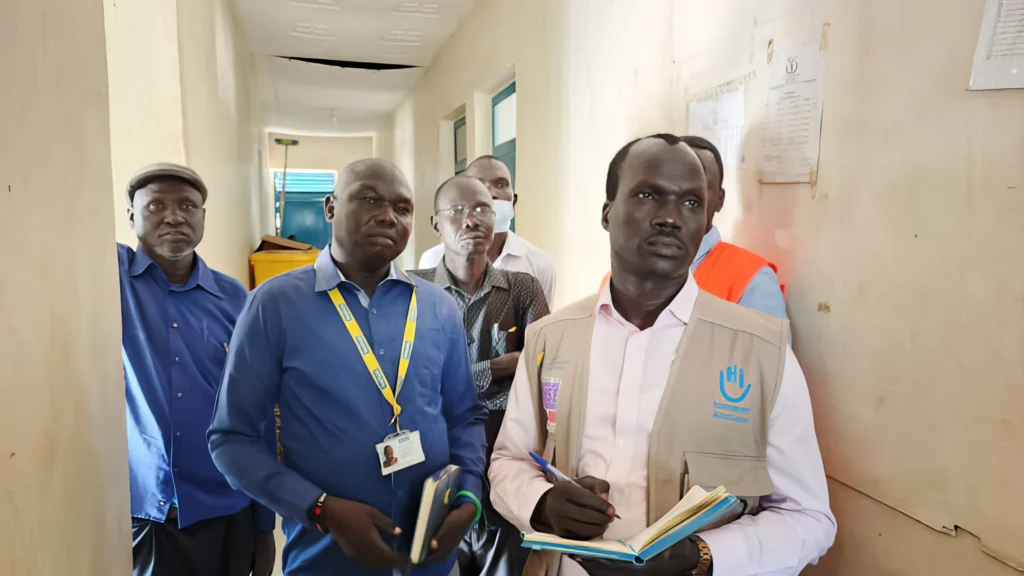
Background: Text to come. Credit:
In 2020, a single outbreak of deadly infectious disease travelled around the world, changing life as we know it. But every year, there are many near misses—outbreaks that are successfully controlled before they become epidemics.
These Epidemics That Didn’t Happen show how the trajectory of an epidemic can be fundamentally altered when a country invests in and prioritizes preparedness for infectious disease outbreaks and readiness to act when they strike. Through this investment and prioritization, we can save millions of lives and trillions of dollars and avert global tragedy in the years to come.
Latest Case Studies
Flagship reports
Do you know of an epidemic that didn't happen?
If so, we’d love to highlight your story. Please reach out to
info@resolvetosavelives.org