EpidemicsThat Didn'tHappen
Responsive health systems are the bedrock of epidemic prevention.
Latest report
2024
The world was quick to move on from COVID-19, yet ongoing outbreaks and not-so-novel pathogens continue to threaten lives and livelihoods. The cholera pandemic is now well into its seventh decade.1 Malaria and other tropical diseases are making a comeback in places where they were once thought extinguished—and cropping up in places they’ve never been recorded. Avian influenza continues to pose threats to humans across the globe.2 And climate change is now accelerating many of the trends that amplify the risk of further outbreaks.3
Countries around the world are often dealing with multiple urgent health issues—which they’re typically forced to prioritize and solve with tight budgets and limited staff and resources. When they don’t manage to contain an outbreak, everyone pays the price. Preventable illness and death, disruptions to essential health services and economic and social costs reverberate for generations. But every day, around the world, responsive health systems are helping to keep millions of lives and livelihoods safe.
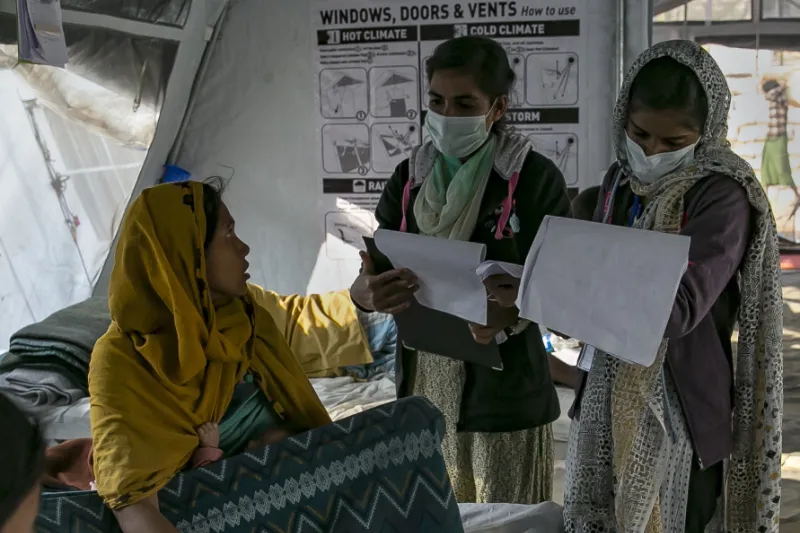
Background: Rohingya refugees being treated by nurses at a diphtheria clinic in Cox’s Bazar, Bangladesh. Credit: Allison Joyce via Getty Images
There is no secret to success when it comes to preventing epidemics. A few simple principles keep health systems prepared to deal with outbreaks quickly and effectively.
This latest edition of Epidemics That Didn’t Happen tells the stories of just some of the recent outbreaks that responsive health systems have stopped in their tracks. It’s easy, and important, to focus on and learn from things going wrong. But it’s just as important to learn from things going right. There is no secret to success when it comes to preventing epidemics. A few simple principles keep health systems prepared to deal with outbreaks quickly and effectively.
Some of the core principles that emerged from these stories include:
Health systems need to listen.
Community immunization campaign in Hasanpur, Haryana, India. Credit: uniquely india via Getty Images

Community immunization campaign in Hasanpur, Haryana, India. Credit: uniquely india via Getty Images
The most effective health systems are sensitive to the needs of the local communities they serve. This means paying close attention to signals provided by local community members and taking appropriate action in response. It also means building deep, ongoing relationships over the years and decades—and not just engaging communities in a crisis. In partnering with communities, health systems build trust that ultimately helps keep everyone safe.

People prevent epidemics.
Doctor explaining dosage and providing medicine to villagers. Credit: Mayur Kakade via Getty Images
Behind every epidemic that didn’t happen are human beings who helped find, report or respond to warning signs. From the farmers who recognized something was wrong with their livestock, to the nurse who reported suspicious symptoms to a district health office, communities play a critical role in both outbreak detection and response efforts and, ultimately, keeping themselves and each other safe.
Timeliness is key.
A veterinarian vaccinates a cow against anthrax. Credit: PERO studio/Shutterstock

A veterinarian vaccinates a cow against anthrax. Credit: PERO studio/Shutterstock
Quite simply, outbreaks stop sooner and do less damage when people act quickly to detect, report and respond to the first signs of a potential threat. To ensure outbreaks are stopped quickly, health systems need committed leaders at all levels and strong collaborations across different sectors—plus access to emergency funds to enable effective action in those critical early days. Making sure response efforts happen as soon as possible saves lives—and the 7-1-7 target is designed to support health systems with achieving this goal.4

Climate change is exacerbating risks.
A man wades through a flooded road in Chattogram, Bangladesh. Credit: Xinhua News Agency via Getty Images
Many outbreaks featured in this year’s report were associated with severe weather events including cyclones and flooding, events that are expected to become more common in many areas already prone to outbreaks. By paying attention to upstream signals that indicate a surge in infectious disease is imminent, like unseasonal rain or heavy flooding, responsive health systems can offset some of these heightened risks.
These stories show that preparedness works. We can prevent epidemics, save lives and protect livelihoods.
Being responsive is a cornerstone of good preparedness—and collectively, these stories show that preparedness works. The trajectory of an outbreak is fundamentally different when a country has invested in preparedness and stands ready to act when infectious disease strikes. We can prevent epidemics, save lives and protect livelihoods.
THESE ARE A FEW OF THE EPIDEMICS THAT DIDN’T HAPPEN Over the last year:

Lassa Fever
GHANA
Government health authorities made skillful use of emergency funds to rapidly contain an outbreak.

Avian Influenza
Finland
Human and animal health authorities joined forces to bring an outbreak under control with no human cases.

Dengue Fever
Somalia
Local community volunteers worked with public health experts to protect themselves and their neighbors.

Cholera
Bangladesh
Decades of effort paid off when a successful response prevented an outbreak from exacerbating a refugee crisis.

Neethling disease
CAMBODIA
Against a backdrop of an ongoing epidemic in livestock, forest rangers prevented cases spreading to endangered wildlife.

Leptospirosis
VANUATU
Despite being hit by two cyclones that wrecked critical infrastructure, health agencies minimized disease spread and protected communities.

conclusion
References
- Deen, J. et al. (2020). Epidemiology of cholera. Vaccine, 38 (1), 31-40. https://doi.org/10.1016/j.vaccine.2019.07.078
- Nolen, S. (2024). The Disease Detectives Trying to Keep the World Safe From Bird Flu, The New York Times. https://www.nytimes.com/2024/05/20/health/bird-flu-tracking-cambodia.html
- NASA. How does climate change affect precipitation? https://gpm.nasa.gov/resources/faq/how-does-climate-change-affect-precipitation
- 7-1-7 Alliance. What is 7-1-7? https://717alliance.org/#faqs