EpidemicsThat Didn'tHappen
These stories show that we can prevent epidemics, saving lives and protecting livelihoods.
The threat of a new or known infectious disease outbreak is constant. But this report demonstrates that these threats can be stopped. These stories show how responsive health systems, in partnership with communities, acting quickly with available funding, and paying attention to signals, can fundamentally alter the trajectory of an outbreak.
These stories provide important lessons for health systems aiming to emulate these successes, including:
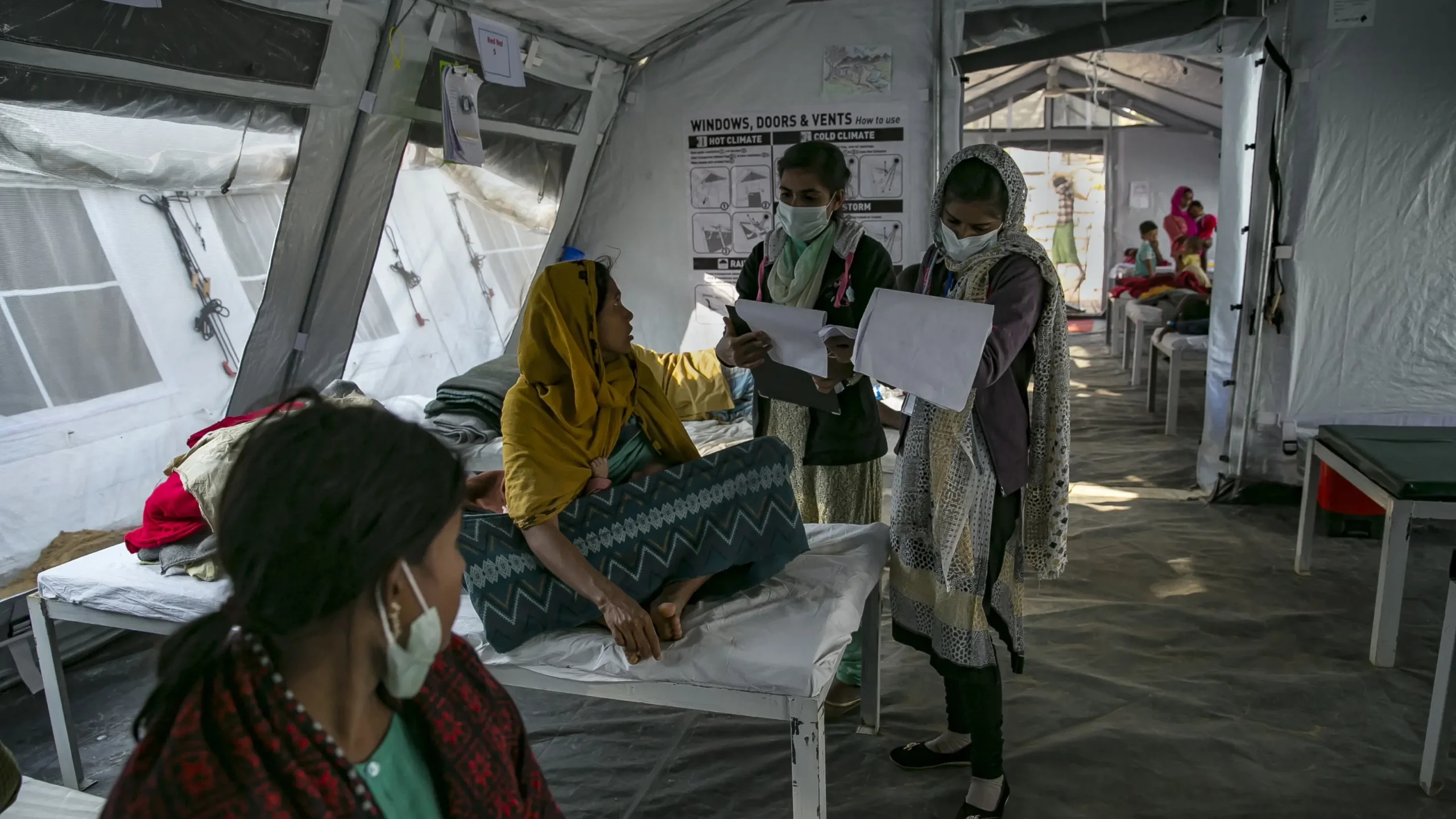
Header: A Rohingya refugee at the Nayapara Refugee Camp in Cox’s Bazar. Credit: MUNIR UZ ZAMAN via Getty Images
Be responsive to communities.

People walk through a marketplace in a Rohingya refugee camp in Cox’s Bazar, Bangladesh. Credit: Allison Joyce via Getty Images
Health systems can only be responsive to communities if they have long-lasting relationships, fit-for-purpose technology systems that allow them to receive early signals, and funding to get response activities off the ground. Even $5,000 of early, flexible funding skillfully allocated in the very first signals of an outbreak can stop an epidemic in its tracks. Primary health facilities are often the first point of contact with the health system: they must be fully supported to fulfill this essential role. We learned about the benefits of responsive communities in these case studies:
- Lassa fever in Ghana: early access to emergency funds enabled a rapid response effort
- Avian influenza in Finland: a surveillance system allowed a concerned farmer to sound the alarm
- Neethling disease in Cambodia: partnering with rangers and vets protected endangered wildlife
People walk through a marketplace in a Rohingya refugee camp in Cox’s Bazar, Bangladesh. Credit: Allison Joyce via Getty Images

Make timeliness a priority.
7-1-7 is a global timeliness target promoting early and effective action to contain infectious disease outbreaks. The 7-1-7 target includes clear performance standards for three timeliness metrics—7 days to detect a suspected disease outbreak, 1 day to notify relevant public health authorities and 7 days to complete early response actions—that enable health systems to stop outbreaks as quickly as possible and minimizing their impact on livelihoods and lives. We saw how timeliness saves lives and economies in these case studies:
- Avian influenza in Finland: authorities responded the day they received a sample from a farmer
- Dengue fever in Somalia: the response team arrived in the village just two days after the report
- Cholera in Bangladesh: a team was deployed to investigate every reported case within 24 hours
Protect health care workers.

Strong infection prevention and control (IPC) programs are a cornerstone of health care delivery and essential for keeping health care workers, patients, and communities safe. Every country needs its own dedicated domestic IPC budget to make sure its health care workers can work with the dignity they deserve in safe facilities, minimizing their exposure to avoidable infections and providing them the equipment and skills needed to stay safe while protecting the rest of us. These case studies highlighted the importance of protecting health care workers so they can protect communities:
- Lassa fever in Ghana: quarantining and treating an infected health worker led to a full recovery
- Avian influenza in Finland: health workers treating suspected cases were protected with PPE
- Leptospirosis in Vanuatu: workers visiting affected communities were trained how to stay safe
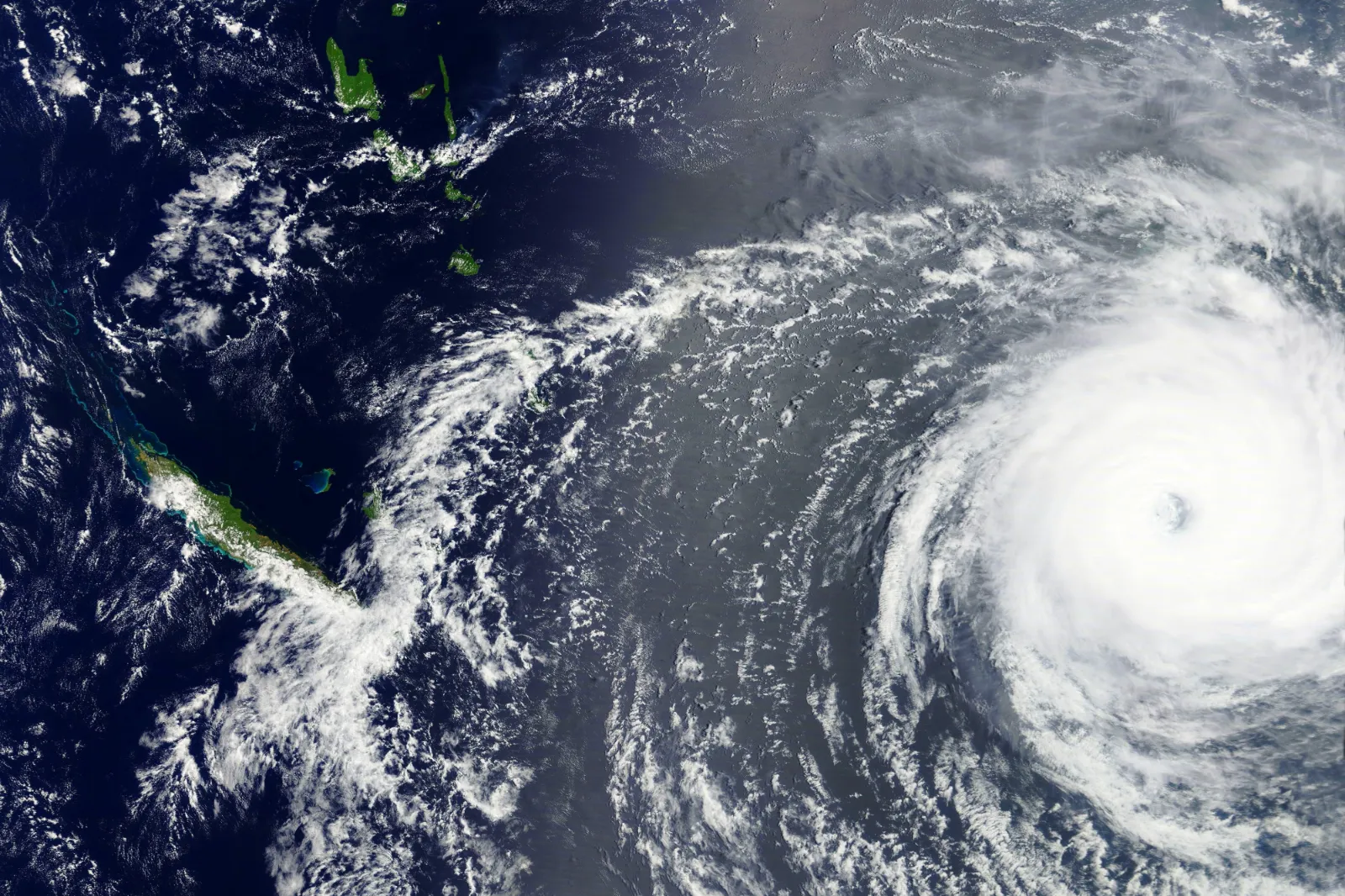
Pay attention to climate signals.
There are many indicators suggesting an increased risk of an outbreak well before a first case has even been found. Such early-warning approaches include paying attention to predictable seasonal shifts (like rainy season) and more sporadic triggers (like cyclones), upstream signals that could be the key to stopping an outbreak before it can start. It is critical for health systems to be responsive to such signals if they wish to overcome the heightened threats posed by climate change. We saw the role of climate in these case studies:
- Dengue fever in Somalia: stronger rains driven by El Niño suggest more mosquito breeding sites
- Cholera in Bangladesh: unusual heavy rains led to predictable flooding and contaminated water
- Leptospirosis in Vanuatu: tracking impending cyclones allowed officials to prepare a response
Responsive health systems are the bedrock of epidemic prevention.
By making strides to prioritize and act on these important lessons, decisionmakers can work towards health systems that are more responsive and better prepared to deal with outbreaks quickly and decisively. Health systems must remain adaptive to the shifting circumstances of the world around us, so they can respond to the changing needs of their communities, and ultimately do their part to save lives and protect livelihoods. The astute communities and public health experts in this report show that this is possible and should be celebrated.